The most recent (updated February 2024) Wilderness Medical Society Practice Guidelines, Tactical Combat Casualty Care and Prolonged Field Care Clinical Practice Guidelines, and other references related to the care of patients in austere environments with PDF links when available.
Wilderness Medical Society Practice Guidelines
and other related materials
The Wilderness and Environmental Medicine Journal The journal of the Wilderness Medical Society. Membership in the WMS gives you access to the most recent journal articles but non-members can read everything other than the most recent journal edition (meaning you can wait and read them when they become open access).
Wilderness First Aid Scope of Practice Minimum Guidelines and Scope of Practice for Wilderness First Aid
Wilderness First Responder Scope of Practice Minimum Guidelines and Scope of Practice for Wilderness First Responder
Water Treatment: 2024 Update Wilderness Medical Society Clinical Practice Guidelines for Water Disinfection for Wilderness, International Travel, and Austere Situations: 2024
Spinal Cord Protection: 2024 Update Wilderness Medical Society Clinical Practice Guidelines for Spinal Cord Protection: 2024 Update
NEXUS vs Canadian C-Spine Rules The New England Journal of Medicine, The Canadian C-Spine Rule versus the NEXUS Low-Risk Criteria in Patients with Trauma
Hemorrhage Control I Application of Current Hemorrhage Control Techniques for Backcountry Care: Part One, Tourniquets and Hemorrhage Control Adjuncts: 2015
Hemorrhage Control II Application of Current Hemorrhage Control Techniques for Backcountry Care: Part Two, Hemostatic Dressings and Other Adjuncts: 2015
Acute Pain Management Wilderness Medical Society Practice Guidelines for the Treatment of Acute Pain in Remote Environments: 2014
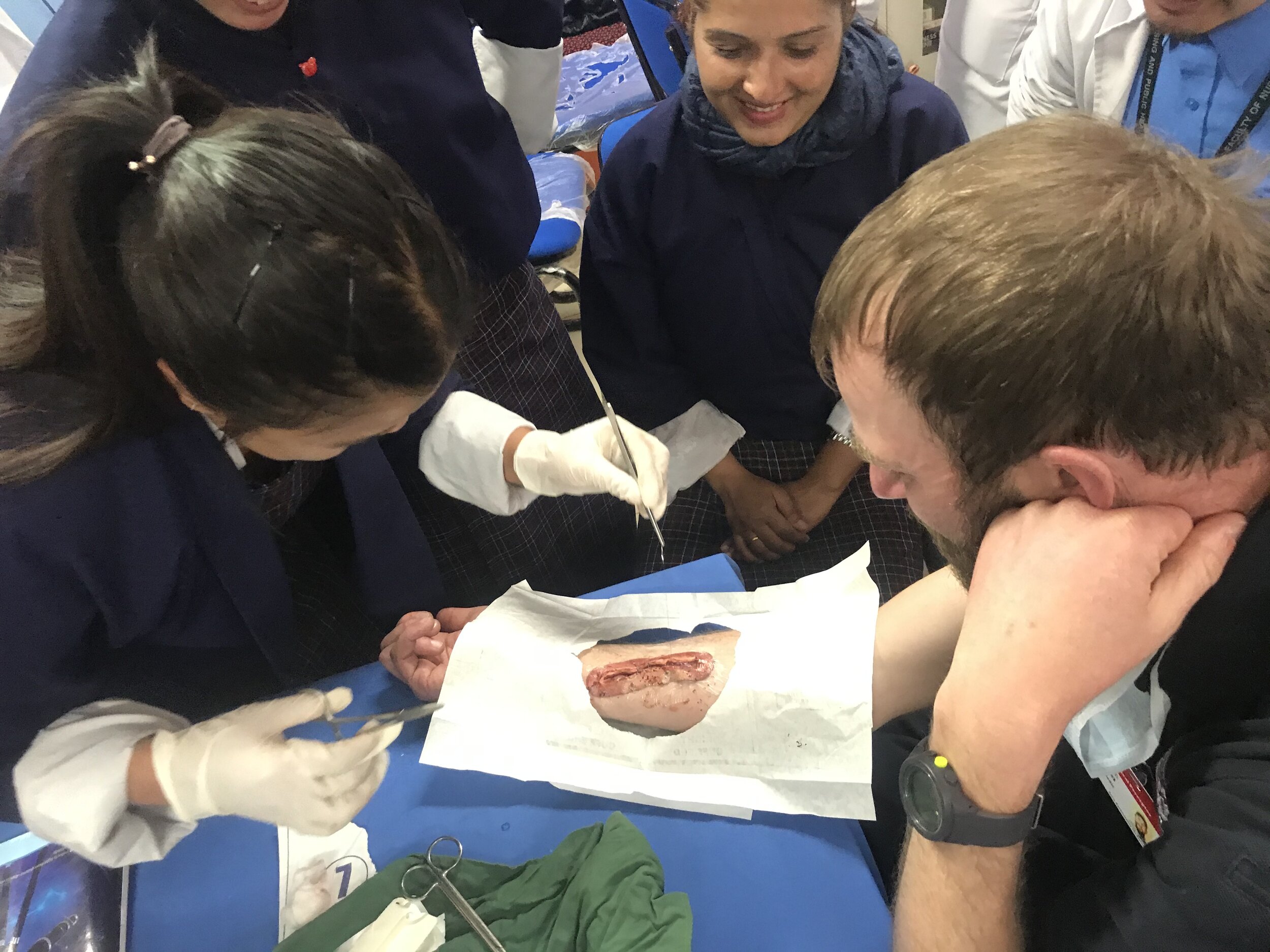
Basic Wound Care Wilderness Medical Society Practice Guidelines for Basic Wound Management in the Austere Environment: 2014
Burn Care Management of Burn Injuries in the Wilderness: Lessons from Low-Resource Settings: 2016
Eye Injuries Wilderness Medical Society Practice Guidelines for Treatment of Eye Injuries and Illnesses in the Wilderness: 2014
Hypothermia Treatment and Prevention Wilderness Medical Society Practice Guidelines for the Out-of-Hospital Evaluation and Treatment of Accidental Hypothermia: 2019 Update
Hypothermia Information Card “Cold Card” to Guide Responders in the Assessment and Care of Cold-Exposed Patients
Hypothermia and Afterdrop Hypothermia Evidence, Afterdrop, and Guidelines
Hypothermia Wrap Comparisons Human Responses to 5 Heated Hypothermia Wrap Systems in a Cold Environment
Head and Torso Rewarming Efficacy of Head and Torso Rewarming Using a Human Model for Severe Hypothermia
Burn Risk from Rewarming Methods Risk of Burns During Active External Rewarming for Accidental Hypothermia
Cold Water Immersion Case Review Problems and Complications With Cold-Water Rescue
Frostbite Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Frostbite: 2019 Update
Nonfreezing Cold Injuries and Warm Water Immersion Tissue Injuries Prevention and Treatment of Nonfreezing Cold Injuries and Warm Water Immersion Tissue Injuries: Supplement to Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Frostbite: 2023
Heat Illnesses Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Heat Illness: 2019 Update
Exertional Heat Stroke Consensus Statement - Prehospital Care of Exertional Heat Stroke
Exercise-Associated Hyponatremia Wilderness Medical Society Practice Guidelines for the Management of Exercise-Associated Hyponatremia: 2019 Update
Anaphylaxis Wilderness Medical Society Practice Guidelines on Anaphylaxis: 2022
Epinephrine Administration Wilderness Medical Society Practice Guidelines for the Use of Epinephrine in Outdoor Education and Wilderness Settings: 2014
Anaphylaxis World Allergy Organization Anaphylaxis Guidance: 2020
Diabetes Management Wilderness Medical Society Clinical Practice Guidelines for Diabetes Management: 2019
Lightning Treatment and Prevention Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Lightning Injuries: 2014
Backcountry Lightning Risk Management Lightning Risk Management for Backcountry Campers and Hikers
Drowning: 2024 Update Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Drowning: 2024 Update
Drowning, Definition and Controversies Drowning in a Sea of Misinformation: Dry Drowning and Secondary Drowning
Management of Avalanche Victims: 2024 Update Wilderness Medical Society Practice Guidelines for Prevention and Management of Avalanche and Nonavalanche Snow Burial Accidents: 2024
Altitude Illnesses: 2024 Update Wilderness Medical Society Practice Guidelines for the Prevention, Diagnosis, and Treatment of Acute Altitude Illness: 2024 Update
North American Pit Viper Envenomations Wilderness Medical Society Practice Guidelines for the Treatment of Pitviper Envenomations in the United States and Canada: 2015
Tick-Borne Illness in the United States Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Management of Tick-Borne Illness in the United States: 2021
Tick-Born Diseases of the United States A CDC Reference Manual for Healthcare Providers (excellent educational photos; includes tick-borne disease abroad): 2018
Canyon Incidents International Commission for Mountain Emergency Medicine Consensus Guidelines for On-Site Management and Transport of Patients in Canyoning Incidents: 2018
Tactical Combat Casualty Care Guidelines
Deployed Medicine “Deployed Medicine is a platform used by the Defense Health Agency to trial new innovative learning models aimed at improving readiness and performance of deployed military medical personnel. The intent is to deliver personalized, dynamic learning using the most current and accessible technology, enabling a self-directed and continuous study of medical best practices and lessons learned.” The central site which includes all TCCC and Joint Trauma System Clinical Practice Guidelines. LOTS of resources for learning and teaching including videos.
Tactical Combat Casualty Care
Tactical Combat Casualty Care TCCC Guidelines for Medical Personnel (Basic Management Plan for Care Under Fire, Tactical Field Care, and Tactical Evacuation Care): 25 January 2024
Tourniquets and Tourniquet Conversion 2023 Includes tourniquet replacement and conversion guidelines and instructions. Unable to link direct PDF, you may need to register on deployedmedicine.com to view information and instructional videos.
TCCC-Medical Provider Guidelines and Curriculum
Tourniquets, Hemostatic Dressings, Junctional Tourniquets, Airway Management C0TCCC Recommended Devices and Adjuncts as of: 01 September 2021
Prolonged Field Care/Prolonged Casualty Care Clinical Practice Guidelines
Prolonged Field Care The site of the Prolonged Field Care working group and podcast. LOTS of great resources including teaching aids.
Prolonged Casualty Care Guidelines (CPG ID: 91) The Prolonged Casualty Care (PCC) guidelines are a consolidated list of casualty-centric knowledge, skills, and best practices intended to serve as the DoD baseline clinical practice guidance to guide casualty management over a prolonged amount of time in austere, remote, or expeditionary settings, and/or during long-distance movements. 21 December 2021
Acute Traumatic Wound Management in the Prolonged Field Care Setting (CPG ID: 62) The intent of this guideline is to provide evidence- and experience-based solutions to those who manage both simple and complex wounds in an austere environment: 2017
Airway Management in Prolonged Field Care (CPG ID:80) This Role 1, prolonged field care (PFC) clinical practice guideline (CPG) is intended to be used after Tactical Combat Casualty Care (TCCC) Guidelines, when evacuation to higher level of care is not immediately possible: 2020
Analgesia and Sedation Management During Prolonged Field Care (CPG ID: 61) The intent of this guideline is to identify potential issues one must consider when providing analgesia with or /without sedation for an extended time. This guideline begins where Tactical Combat Casualty Care (TCCC) guidelines end: 2017
Burn Wound Management Under Prolonged Field Care (CPG ID: 57) This Role 1 prolonged field care (PFC) guideline is intended to be used after Tactical Combat Casualty Care (TCCC) Guidelines, when evacuation to higher level of care is not immediately possible: 2017
Crush Syndrome Under Prolonged Field Care (CPG ID: 58) This Role 1 prolonged field care (PFC) guideline is meant to provide medical professionals who encounter crush syndrome in austere environments with evidence-based guidance for how to manage the various aspects of crush injury care and monitoring: 2016
Damage Control Resuscitation (DCR) in Prolonged Field Care (CPG ID:73) The purpose of this guideline is to improve implementation of DCR in the Role 1 PFC environment.
Documentation in Prolonged Field Care (CPG ID:72) This CPG is meant to provide medical professionals who treat severely injured or sick patients in austere environments with recommendations for documentation that will allow them and subsequent providers along the evacuation chain to optimally manage complex, often unstable casualties: 2018
Management of COVID-19 in Austere Operational Environments (Prehospital & Prolonged Field Care), 23 Apr 2021
Nursing Intervention in Prolonged Field Care (CPG ID: 70) The intent of this guideline is to provide medical professionals who encounter extended casualty evacuation times in austere environments the evidence-based guidance for nursing interventions necessary to improve patient outcome: 2018
Ocular Injuries and Vision-Threatening Conditions in Prolonged Field Care (CPG ID: 66) This guide provides medical professionals with essential information on the recognition and treatment of ocular conditions when evacuation to an eye specialist is delayed: 2017
Sepsis Management in Prolonged Field Care (CPG ID: 83) Focuses on the most common etiologies of sepsis, and the treatments of those forms of sepsis that the austere provider can reasonably manage.
Traumatic Brain Injury Management in Prolonged Field Care (CPG ID: 63) This CPG provide medical professionals who encounter traumatic brain injury (TBI) in austere environments with evidence-based guidance: 2017
En Route Combat Casualty Care
Basic Management Plan for Tactical Evacuation Care No pdf, direct link.
Interfacility Transport of Patients Between Theater Medical Treatment Facilities This JTS CPG recommends the minimum requirements and capabilities for the movement of critical care patients between medical treatment facilities (MTFs): 2018 No pdf, direct link.
CCAT iSTAT Use Clinical Practice Guideline This guideline establishes expectations for maintenance, calibration and quality control of the iSTAT portable blood analyzer.
Prehospital Blood Transfusion (CPG ID:82) The CPG provides a brief summary of the scientific literature for prehospital blood use and essential instructions on resuscitation procedures using blood products.
Joint Trauma System Clinical Practice Guidelines
Acute Extremity Compartment Syndrome (CS) and the Role of Fasciotomy in Extremity War Wounds (CPG ID: 17) Guide providers in the evaluation and treatment of patients with extremity war wounds, including the role of prophylactic and therapeutic fasciotomy: 2016
Acute Respiratory Failure (CPG ID: 6) This CPG describes the associated risk factors, diagnosis, and management of Acute Respiratory Distress Syndrome (ARDS) in combat casualties in the forward deployed environment and the resources available for safe aeromedical transport of these patients: 2017
Airway Management of Traumatic Injuries (CPG: 39) To optimize the airway management for patients with traumatic injury in the operational medical treatment facility environment: 2017
Amputation: Evaluation and Treatment (CPG 07) To provide standardization of optimal care for the performance of wound management and life-saving amputations that will ensure preservation of maximum limb length, promote healing of viable tissues, and facilitate optimal rehabilitative function: 2016
Anesthesia for Trauma Patients A method of anesthesia that incorporates the induction and maintenance of anesthesia into an ongoing resuscitation during surgery for a trauma patient in extremis: 2016
Aural Blast Injury/Acoustic Trauma and Hearing Loss (ID:05) This CPG will help the reader to quickly identify and treat aural trauma and hearing loss, to prevent morbidity, and to preserve as much function as possible – even while in the combat theater: 2018
Battle and Non-Battle Injury Documentation: The Resuscitation Record. 2013
Bites, Stings and Envenomation (CPG ID: 60) This CPG provides an overview of bites, stings and envenomation and presents a standardized approach to providers in the evaluation and treatment of patients with animal induced trauma and toxins: 2018
Blunt Abdominal Trauma, Splenectomy, and Post-Splenectomy Vaccination (CPG ID: 09) To provide guidance on the management of combat casualties who sustain blunt abdominal trauma: 2016
Burn Care Addresses burn injury assessment, resuscitation, wound care, and specific scenarios including chemical and electrical injuries. Reviews considerations for the definitive care of local national patients, including pediatric patients, who are unable to be evacuated from theater: 2016
Catastrophic Non-Survivable Brain Injury (CPG ID: 13) Useful guidelines to manage casualties with catastrophic, non-survivable brain injury at Role 2 and Role 3 facilities: 2017
Cervical and Thoracolumbar Spine Injury Evaluation, Transport, and Surgery in the Deployed Setting (CPG ID: 15) Guidance for providing the best care to patients who suffer a spine or spinal cord injury: 2016
Chemical, Biological, Radiological and Nuclear (CBRN) Injury Part I: Initial Response to CBRN Agents (CPG ID: 69) This guideline is intended for use in conjunction with Tactical Combat Casualty Care (TCCC) guidelines as an organized approach to the care of chemical, biological, radiological and nuclear (CBRN) casualties in the deployed environment: 2018
Damage Control Resuscitation (CPG ID: 18) This CPG provides evidence–based guidance to minimize variation in resuscitation practices and improve the care of massively hemorrhaging, severely injured casualties: 2019
Drowning Management (CPG ID: 64) This guide helps first responders, prehospital emergency medical service personnel, and medical department personnel evaluate, diagnose and manage common in-water pathologies: 2017
Emergency General Surgery in Deployed Locations (CPG ID: 71) This CPG will guide providers in the evaluation and treatment of patients with acute general surgical needs in potentially austere locations: 2018
Emergency Life-Saving Cranial Procedures by Non-Neurosurgeons in Deployed Setting (CPG ID:68) This CPG applies to military non-neurosurgeons in a forward deployed location with surgical capability (Role 2 surgical teams that meet capability requirements) outside of the United States: 2018
Emergent Resuscitative Thoracotomy (ERT) (CPG ID: 20) Summarizes recommendations and technique for ERT in a Military Treatment Facility (MTF) in a combat or operational environment. The primary goal is to rapidly identify and correct any life threatening pathology and to provide care that results in a survivor with a meaningful level of function and cognition: 2018
Eye Trauma (CPG ID: 03) This CPG provides a step-by-step approach for the non-ophthalmologist in the initial evaluation and treatment of eye trauma injuries sustained in the combat theater or in remote and austere environments: 2021
Frostbite and Immersion Foot Care (CPG ID: 59) This CPG provides an overview of cold injuries and presents a standardized approach to providers in the evaluation and treatment of patients with cold injuries including the role of intravascular therapy: 2017
Frozen and Deglycerolized Red Blood Cells (CPG ID: 26) Provide guidance for the use of frozen and thawed/Deglycerolized Red Blood Cells (DRBCs) in the combat theater: 2016
Genitourinary (GU) Injury Trauma Management (CPG ID: 42) This CPG provides indications for and the procedures associated with the initial management of GU injuries sustained in combat casualties: 2019
High Bilateral Amputations and Dismounted Complex Blast Injury (CPG ID: 22) To review indications for and the procedures associated with the initial management of bilateral lower extremity amputations with associated pelvic/perineal injuries: 2016
Hyperkalemia and Dialysis in the Deployed Setting (CPG ID: 52) Provides recommendations for the management of patients with, or at risk for, acute kidney injury and hyperkalemia in the austere deployed environment: 2017
Hypothermia Prevention, Monitoring, and Management To establish guidance for prevention and management of hypothermia in the combat casualty: 2012
Infection Prevention in Combat-Related Injuries (CPG ID: 24) Provides rationale and guidance for the prevention of infection after combat-related injuries: 2016
Inhalation Injury and Toxic Industrial Chemical Exposure (CPG ID: 25) There are multiple toxic industrial chemicals that act on the respiratory tract. This CPG reviews the most common toxic industrial chemicals related in pulmonary injury: 2016
Initial Care of Ocular and Adnexal Injuries by NonOphthalmologists at Role 1, Role 2, and NonOphthalmic Role 3 Facilities See Eye Trauma above for updated document: 2014
Initial Management of War Wounds: Wound Debridement and Irrigation: 2012
Interfacility Transport of Patients Between Theater Medical Treatment Facilities (CPG ID: 27) This CPG recommends the minimum requirements to move critical care casualties after their entry into the evacuation system: 2018
Invasive Fungal Infection in War Wounds (CPG: 28) Provide guidance on the recognition and comprehensive management of invasive fungal infection (IFI) in war wounds: 2016
Neurosurgery and Severe Head Injury (CPG ID:30) Provides guidelines and recommendations for the treatment and medical management of casualties with moderate to severe head injuries in an environment where personnel, resources and follow-on care may be limited: 2017
Nutritional Support Using Enteral and Parenteral Methods (CPG ID: 33) How to achieve optimal nutritional support for the critically injured or ill patient using enteral nutrition and parenteral nutrition methods: 2016
Orthopaedic Trauma: Extremity Fractures (CPG ID: 56) To describe the initial non-surgical and surgical management of extremity fractures and to define care guidelines for fractures of upper and lower extremities: 2016
Pain, Anxiety and Delirium (CPG ID: 29) This CPG will delineate specific treatment guidelines for pain, anxiety and delirium (PAD) between Role 1, Role 2, Role 3 and higher echelons of care, with an emphasis on Role 3: 2017
Pelvic Fracture Care (CPG ID: 34) Provides a brief review for the stabilization and treatment of pelvic fractures sustained in combat casualties: 2017
Prehospital Trauma Care in the Tactical Setting: 2014
Radiology: Imaging Trauma Patients in a Deployed Setting (CPG ID: 01) Provides general imaging guidelines for Radiologist and Emergency Providers when performing trauma patient assessment in a deployed setting: 2017
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) for Hemorrhagic Shock (CPG ID: 38) Reviews the range of accepted management approaches to profound shock and post-traumatic cardiac arrest and establishes indications for considering REBOA as a hemorrhage control adjunct: 2017
The Prevention of Deep Venous Thrombosis – Inferior Vena Cava Filter (CPG ID: 36) To establish guidance for 1) anti-thrombotic therapy for the prevention of deep venous thrombosis (DVT) and pulmonary embolism (PE) and 2) the management of inferior vena cava filters (IVCs) placed in the combat theater for the purpose of either primary or secondary prophylaxis of pulmonary embolism: 2016
Unexploded Ordnance (UXO) Management (CPG ID: 41) This CPG provides details on the procedures to safely remove unexploded ordnance from combat patients, both loose and impaled, to minimize the risks to providers and the medical treatment facility while ensuring the best outcome for the patient: 2017
Urologic Trauma Management (CPG ID: 42) Provides indications for and the procedures associated with the initial management of genitourinary (GU) trauma sustained in combat casualties: 2017
Use of Electronic Clinical Documentation in the CENTCOM AOR: 2012
Vascular Injury (CPG ID: 46) The CPG provides guidance on the diagnosis, treatment and surgical management of vascular injuries sustained by combat casualties: 2016
Ventilator Associated Pneumonia To establish guidance for the prevention and mitigation of Ventilator Acquired Pneumonia (VAP): 2012
Wartime Thoracic Injury (CPG ID:74) The goal of this CPG is to provide guidance on the diagnosis, initial treatment, and surgical management of thoracic injuries in the deployed or operational environment: 2018
Whole Blood Transfusion (CPG ID: 21) This CPG provides the rationale and guidelines for WB transfusion, including but not limited to product definitions, indications, collection, storage, testing, transfusion, and documentation: 2017
CCAT Temporary Transvenous Pacemaker Clinical Practice Guideline Salma Test: 2018 No pdf available